Ojoo PHC
It was a little past midday at the Ojoo Primary Healthcare Centre (PHC) in Akinyele LGA in Oyo state. Periodically, the loud cry of a woman in labour rose above the hum of voices in the crowded waiting area, where patients sat patiently for their turns to be attended to.
Catherine Adebola, the officer-in-charge (OIC) of the facility, excused herself from the reporter.
“We’re managing a woman in labour. She is having a primie, and I need to step in,” she said.
About ten minutes later, the woman’s cry waned and was replaced by that of a baby. Adebola returned to her office after washing up.
Advertisement
“We have a baby boy. Mother and child are doing fine,” she announced.

The OIC said that thanks to funding from the Basic Healthcare Provision Fund (BHCPF), the centre now has the essential equipment it needs to deliver services — especially antenatal and childbirth care for women.
She explained that when she was deployed to the PHC in 2023, the situation was quite different. Power supply was poor, and during night deliveries, they often had to depend on rechargeable lamps.
Advertisement
“It was terrible,” Adebola recalled.
 Funding from the Basic Health Care Provision Fund (BHCPF) has since altered that reality. The facility now has a 1kVA solar system that powers key areas, including the labour room.
Funding from the Basic Health Care Provision Fund (BHCPF) has since altered that reality. The facility now has a 1kVA solar system that powers key areas, including the labour room.
With an average of 3,000 patients monthly, Ojoo PHC receives ₦300,750 every quarter as Direct Facility Funding (DFF). From this, it has purchased a washing machine for infection control, new chairs, sphygmomanometers, a weighing scale, delivery instruments, laboratory reagents, and registration materials. The facility’s broken borehole, which had been abandoned for two years, was also repaired.
Adebola further said the fund is also expended on power costs, fuel, and other repairs. All these expenses are documented inside the business plan and approved by the state’s healthcare board, she noted.
Advertisement

“The fund has really helped us because in times past, you would not even want to come to this PHC, not because of the staff, but because of the tools to work with. We have now procured a weighing scale, delivery instruments, laboratory reagents and registration cards,” Adebola said.
“I met the borehole faulty when I was deployed here in 2023, but we fixed it in the third quarter of this year from our BHCPF allocation. Before fixing it, we used to buy water from water tanks.
“Now with the BHCPF, we can do some things on our own once we put it inside our business plan. We procure essential drugs like antimalarials and hematinics, and antibiotics and patients under the scheme get the drugs for free.”
As of September, the facility had 1,611 BHCPF enrollees, with 47 treated that month.
Advertisement
AT AYEGUN PHC, WOMEN RETURN BECAUSE ‘THINGS ARE BETTER NOW’
Advertisement
Twenty-three kilometres away, the Ayegun PHC in Akinyele LGA — renovated under the IMPACT Project — tells a similar story of transformation.
For 21-year-old Sakinah Ariyayo, the change is personal. When she delivered her first child at the facility in April 2023, the labour room was lit with candles.
Advertisement
Sakinah had her child at 3.00 am.
“There were only two nurses on duty that night. Even though they had a small solar, it was dim, so we had to light up candles for the delivery,” she said.
Advertisement
“But now, there is light everywhere. I felt encouraged to return for my second pregnancy. I feel very happy. It is a good development. See, now everywhere is well ventilated, we have a lab, good restrooms and drugs.”
The facility now runs basic laboratory tests such as malaria, ANC tests, HIV, hepatitis, syphilis, and PCV. Staffing has also improved, with ten workers, including two CHEWs funded under the BHCPF and a newly recruited night guard.
Although still below the minimum required staffing standard of 24 health workers per PHC, the OIC, simply identified as Mrs Oluwagbemiga, said it has eased workload and reduced waiting time.
Ayegun PHC also receives ₦300,750 quarterly DFF, used for essential drugs, patient records, and utility costs. A solar power system has been installed — critical in a community where electricity barely lasts three hours daily.

WHAT THE BHCPF AIMS TO ACHIEVE
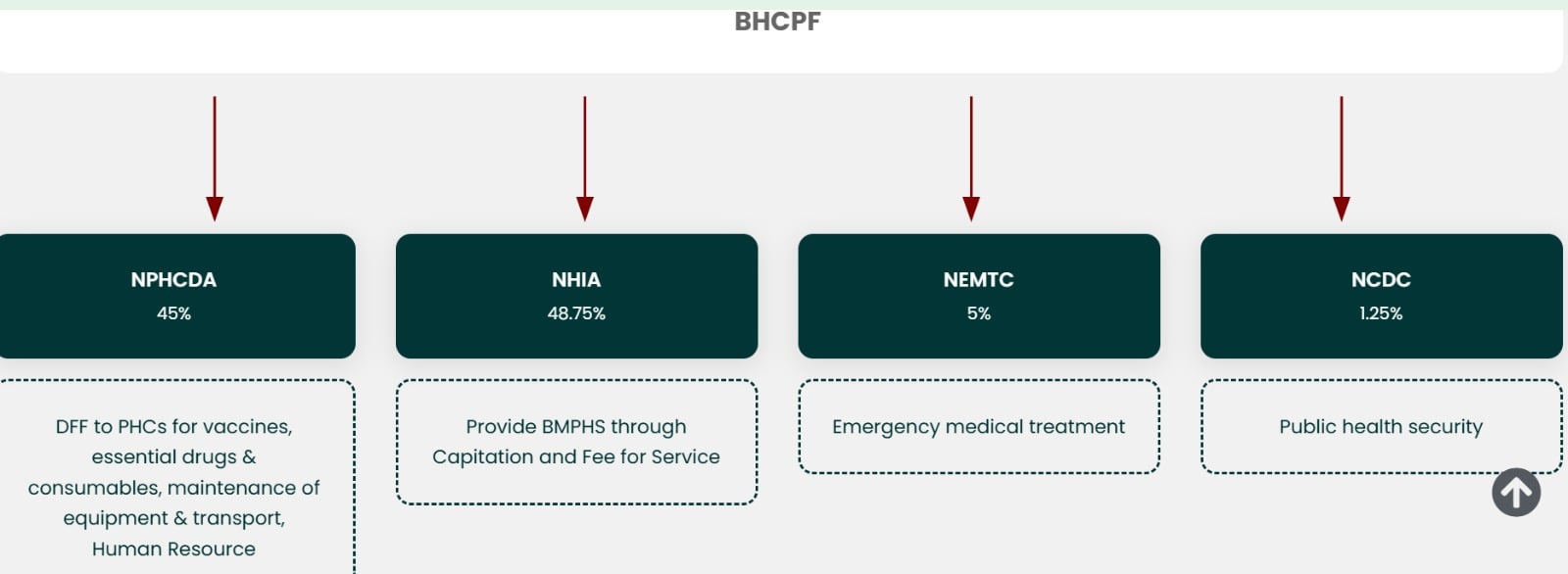
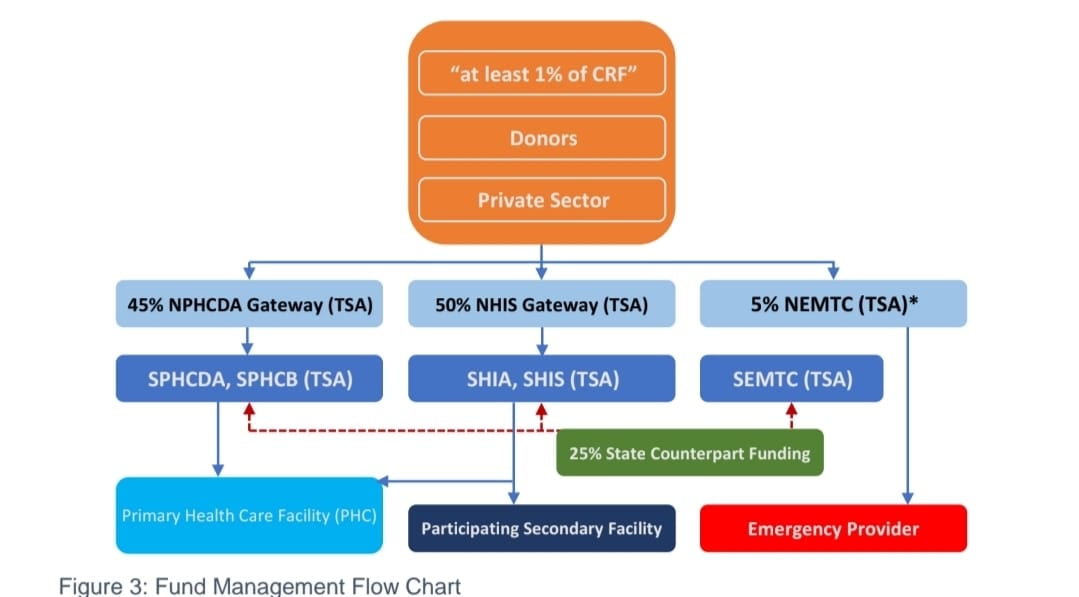
The Basic Health Care Provision Fund (BHCPF), established in Section 11 of the National Health Act 2014 and rolled out in 2019, is Nigeria’s most ambitious primary healthcare reform in decades. Its goal is to finance basic healthcare for the most vulnerable and accelerate the journey towards universal health coverage (UHC).
It is implemented through four gateways — NPHCDA, NHIA, NEMT, and NCDC — and is intended to strengthen PHCs, support emergency services, improve access to essential drugs, and expand health insurance coverage.
By 2027, the federal government aims for 17,600 fully functional PHCs, with at least one in every political ward, and one secondary health facility per LGA benefiting from the fund.
The BHCPF is managed by three key agencies at the national level: the National Primary Health Care Development Agency (NPHCDA), the Federal Ministry of Health, and the National Health Insurance Authority (NHIA).
Every year, the federal government is required to contribute at least 1 percent of its Consolidated Revenue Fund (CRF) to the BHCPF. In addition, individual state governments are required to provide 25 percent of the total funds expected from the BHCPF in counterpart funding as stipulated by section 11 subsections 5a and b of the NHAct 2014. Development partners and international donors also contribute to the fund.
OYO PHCs ONCE IN CRISIS SHOW SIGNS OF RECOVERY
According to the Oyo State Primary Healthcare Board (OYOPHCB), there are over 760 PHCs in the state, out of which 351, through the one facility per ward policy, receive funding from the BHCPF.
In March 2023, the Oyo state government announced that over 200 PHCs in the state will be renovated and upgraded by 2025. Seyi Makinde, the governor, promised that each of the 351 wards in the state would have at least one Grade 3 PHC.
The IMPACT Project was then launched, and at least, 264 PHCs have since been renovated/revitalised across the 33 LGAs in the state.
Subsequently, Makinde, on March 7, 2023, presented a symbolic cheque of N4.5 million to Ward Development Committee (WDC) members for equipping 264 primary healthcare centres across the state.
Eight PHCs per LGA in all 33 LGAs were equipped with medical, laboratory and clinical equipment.
The funding for equipping the PHCs was from the Oyo state government, OYOPHCB, IMPACT Project, and BHCPF.
According to the state government, OYSHIA increased enrollees from 69,996 in September 2019 to 180,048 in September 2023 and 255,140 in May 2025.
TheCable visited some of the revitalised and equipped PHCs to ascertain their levels of functionality and service delivery.
A 2024 report documented severe understaffing at Adifase PHC in Ibadan South-West LGA, where one heavily pregnant health worker managed the facility serving over 700 patients monthly.

During a follow-up visit on October 17, 2025, the situation had significantly improved. TheCable observed the facility had at least four nurses on duty.
The OIC, Adeyemo H.O., confirmed the positive turnaround since she was posted to the facility in December 2024. She acknowledged that before the improved staffing levels, workers at the facility were severely overstretched, such that they ran a 12-hour shift instead of 8 hours.
“We used to run two shifts — 7 am to 7 pm — instead of the standard three. Staff would break down, but now that challenge is gone,” the OIC explained.

“More hands were employed in May,” Adeyemo said, adding that “we now have enough CHEWs, nurses, and community health workers”.
Adeyemo declined to disclose the exact number of health workers at the facility, saying she is not permitted to disclose such details under civil service rules.
The facility also gets the same N300,750 in DFF and over N600,000 in capitation funds from the BHCPF.
“We can see the changes in service delivery, getting drugs for the patients. It has helped us to deliver quality healthcare services to our patients,” she said.
At the Ido PHC in Ido LGA, Oladosu Vincent, the technical coordinator, said the revitalised facility now attracts even “elite” residents because the improvements are visible.
He noted that the PHC is now better positioned to handle the growing number of patients, adding that the improved condition of the facility has restored public confidence.


“Even the elite now use this facility. If it wasn’t in good shape, they wouldn’t come; they would prefer to return to town. But what they’re looking for in town is already here,” Vincent said.
According to Vincent, funding through the BHCPF has further boosted both service delivery and staff welfare.
“The fund has increased both input and output. It has made our staff very comfortable. Before now, it was like working under duress. Before, you would find only three staff in a clinic like this. Now, we have enough personnel to run the facility round the clock,” he noted.
“Today is our immunisation day, and the nursing mothers who came for routine immunisation are not less than 200.”
Babatunde Sekinat, a 43-year-old mother of three, said that when she first gave birth seven years ago, the facility had no running water, only one building, and a few nurses.
“But now, everything has changed. Now, there are many nurses, and I enjoy the experience better; that is why I’m back, Sekinat said.

COMMUNITY INVOLVEMENT THROUGH WDC
The Ward Development Committee (WDC) was holding a meeting at 11 am when TheCable arrived at Adaramagbo PHC in Oluyole LGA on November 3.
BHCPF-affiliated facilities are mandated to have functional WDCs and submit business and quality improvement plans.
Emiade Olabisi, the technical coordinator, took TheCable on a tour of the facility and introduced some members of the WDC who were seated in a meeting room.

“We’re having a meeting with the WDC to inform them of the activities at this health facility. You can see we are running an inclusive and transparent system,” Olabisi said.
Present at the meeting were the supervisory council for health, Oluyole LGA; education secretary for the LGA; Sanusi Adeola, Oyo state internal auditor for IMPACT; and the WDC chairman. Others were representatives from the youth, religious leaders and traders.
“The people you are seeing here are the community, where you have the religious and traditional leaders, youths, and market women. We are all stakeholders,” Adeola said.
“Impact Project came to reduce infant mortality and to extend the scope of health services, and we have done a lot. We have quarterly meetings to get feedback from the people – where are we, where are we going to, are we actually getting there?”
TheCable also met the WDC in a meeting at Ojoo PHC on November 5.
THE WEAK LINKS: GAPS, DELAYS AND THE REALITIES INSIDE STRUGGLING PHCs
Despite the renewed energy flowing into Oyo state’s primary healthcare system, not every facility reflects the basic standards set by the NPHCDA. Across several LGAs, TheCable found pockets of decline – healthcare centres where the promise of the BHCPF is slowed by low awareness, weak infrastructure, and delayed enrolment.
When TheCable arrived at Oke Bola PHC in October, Ogunsowo, a matron who doubles as the OIC, refused to speak on the state of activities at the facility, asking the reporter to get approval from the state government.
However, in the waiting area, TheCable observed an elderly man who had come to get his blood sugar level tested. One of the health workers told the patient that the glucometer was not functioning at the time.
“The last time it got spoilt, I was the one who fixed it,” she said, adding that the device frequently breaks down and needs to be replaced.
At Ayegun PHC, for instance, many beneficiaries still do not fully understand the scheme or the services they are entitled to. Some residents continue to patronise traditional birth attendants, unsure of what the BHCPF offers.
The facility’s OIC said that some enrollees have never returned to the PHC after registering, preferring to self-medicate rather than spend money on transportation.
“During the registration of new BHCPF enrollees, many thought it was a political initiative and expected money to be shared. People even travelled long distances to enrol,” she said.
Other centres face more structural challenges. At Akinyele PHC in Moniya, the facility began receiving BHCPF in the first quarter of 2025. However, the absence of registered beneficiaries means the money goes strictly into repairs and equipment — yet the surroundings remain harsh and unfriendly for patients. A bushy walkway and an exposed waiting area leave expectant mothers at the mercy of the weather.


Amos Ademola, the WDC chairman for Moniya PHC, stated that the committee had engaged the OYOPHCB on the issues but received no response.
“We have been expecting them to do that. In fact, the MOH has an office here with us, but we don’t know what is happening. I have written to the executive secretary, and even the governor, but I have not seen anything for three months now,” Ademola said.
TheCable also discovered equipment shortages that undermine service delivery. At Adifase PHC, the labour couch is barely functional.

“We’re just managing it,” Adeyemo said, adding that a request to purchase a new one has been added to the facility’s business plan for the last quarter of the year.
She also said the facility needs cleaners and health attendants, and urgently needs additional delivery instruments to prevent cross-contamination between patients, especially those living with HIV or hepatitis B.
“For now, when they come in, we use our discretion and sometimes improvise with a blade to separate the placenta from the mother and child instead of scissors because we don’t want to spread the infection,” she explained.
With poor power supply and no solar alternative, laboratory services are often delayed, leaving staff to rely on inconsistent generator use.
Across several PHCs visited, the complaints were consistent: the absence of ultrasound machines, insufficient medical officers, and slow approval processes that delay essential purchases. The gaps reveal the unevenness of BHCPF implementation — a system that works impressively in some wards but struggles to take root in others.
WHAT THE STATE GOVERNMENT IS SAYING
When TheCable presented its findings to the Oyo State Primary Healthcare Board (OYOPHCB), Biodun Akande, the director of special duties, who spoke on behalf of Muideen Olatunji, the executive secretary, said the state has made “significant improvements” since it began receiving BHCPF allocations in 2020.
According to Akande, Oyo state has received over N3 billion (₦3,072,422,452) from the federal government, while the state government has contributed ₦100 million in counterpart funding within the same period. He said the state is using the fund to close critical gaps — strengthening the drug revolving fund (DRF), improving 24/7 service delivery at primary healthcare centres (PHCs), and reducing out-of-pocket healthcare expenses for vulnerable residents.
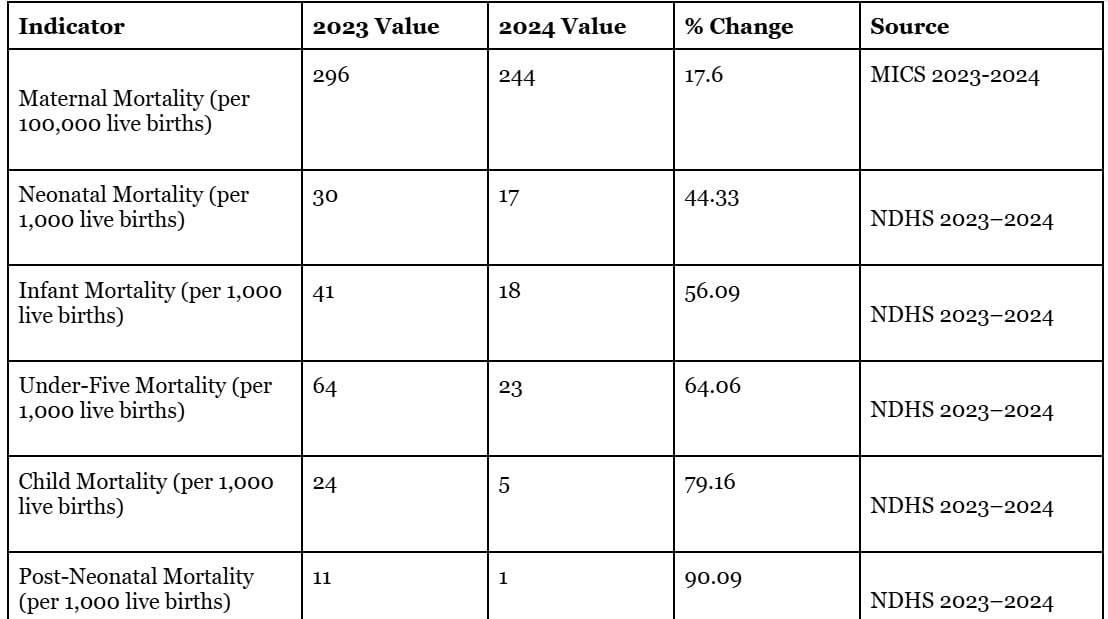
“How do I know we’re moving forward? I compared the 2020 scorecard with what we have now,” he said.
“Most of the health indices that were in red have shifted to yellow, and some to green. So, I can say categorically that we have recorded improvements.”
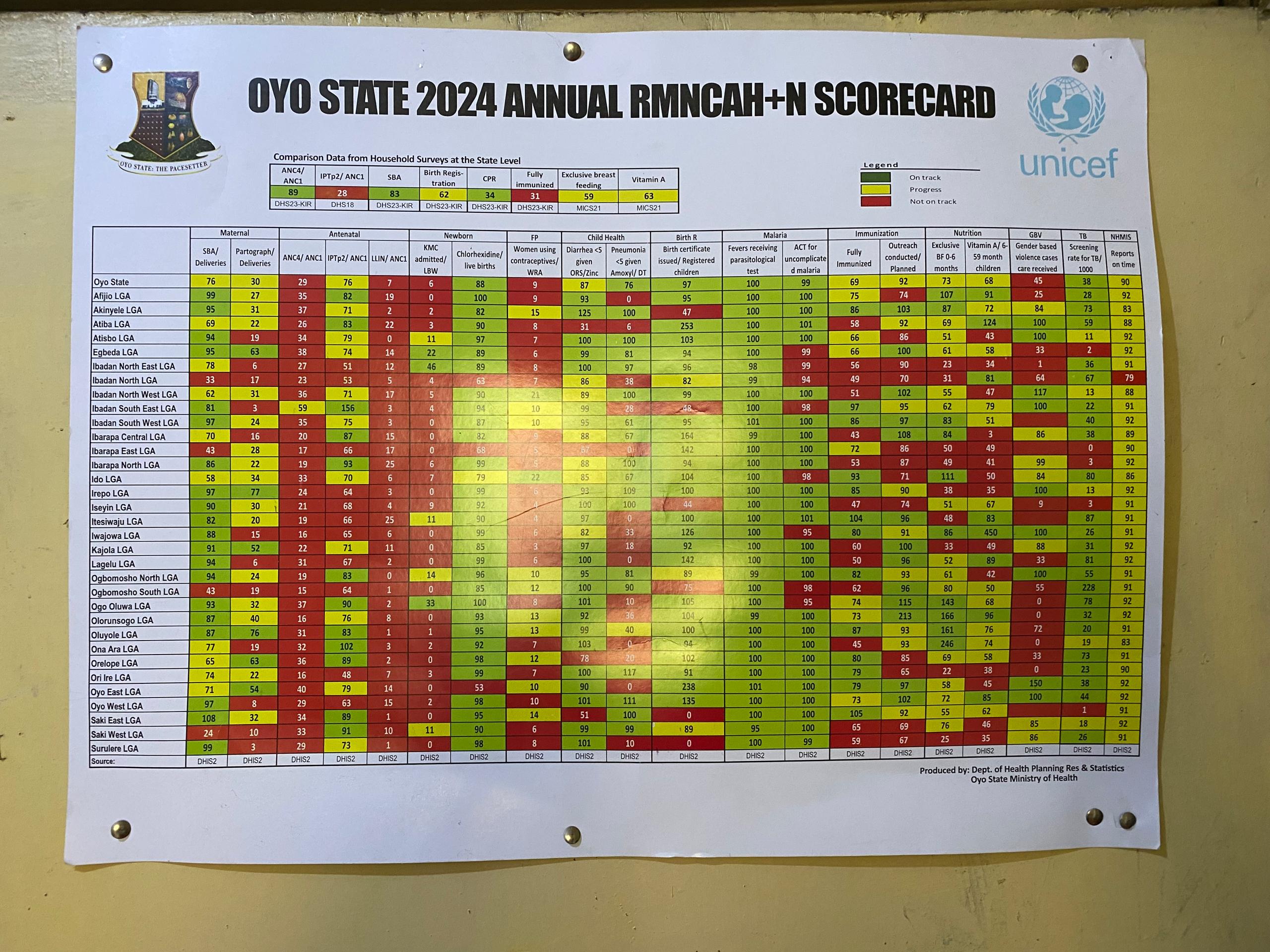
Akande explained that 109,156 people have so far been enrolled under the BHCPF in Oyo, almost double the original target of 60,000 set at the launch of BHCPF 1.0. With BHCPF 2.0 underway, the state plans to expand further, adding 137 more facilities over the next four to five years.
On accountability, he said the state monitors how PHCs use their facility financing through WDCs, regular integrated supportive supervision visits, and routine meetings with health workers. The state has also launched a whistleblower policy to strengthen transparency.
He described the flow of funds as tightly regulated: “If we don’t get approval from the federal government, we cannot disburse. Every year, we prepare a plan with the national authorities. When approval comes, funds go into a CBN domiciliary account, then into Oyo’s Treasury Single Account (TSA). We wait for approval to spend before disbursing to facilities. PHCs would have prepared their business plans and submitted them for approval as well.”
On the scarcity of scanning machines and the low number of doctors, Akande said the government is making gradual progress.
“We plan for each LGA to run scan services. We’ve started in three LGAs but haven’t completed the rollout. Some LGAs even have machines that are yet to be activated,” he said.
Asked whether the government is considering portable scanning machines to bridge the gap, Akande said the option “will be considered and test-run in some PHCs”.
As for medical personnel, he said the state has increased its doctor workforce, and that between 2024 and 2025, the state government recruited 3,980 health workers, with the process beginning in 2024.
“The first batch was recruited in March 2025, and the exercise was completed in June,” he said.
“We recruited 44 new doctors in addition to the 17 we had. So now, each LGA has about two doctors who rotate across facilities rather than being stationed in one centre.”
This report was made possible with support from the International Centre for Investigative Reporting (ICIR) under its Strengthening Public Accountability For Results and Knowledge (SPARK 2.2) project.