Kyuntu John walks toward the spot where she will board a motorcycle to the junction, from where she will take a cab to the Lugbe Primary Health Care Centre in Abuja, Nigeria, where she collects her antiretroviral therapy (ART) medication. July 29, 2025. Photograph: Marvellous Durowaiye /CCIJ
BY BELOVED JOHN
Kyuntu John, a mother of three, is running out of her antiretroviral drugs needed to fight AIDS. In a matter of days, her supply will end. But in the wake of the Trump administration’s massive cuts of billions of dollars in international assistance, she is among many Africans facing a hard time getting resupplied with needed medications.
President Donald Trump froze almost all U.S. foreign assistance as one of his first acts in office. Despite legal challenges and a promise to resume “life-saving humanitarian assistance,” programs in Nigeria remain seriously disrupted.
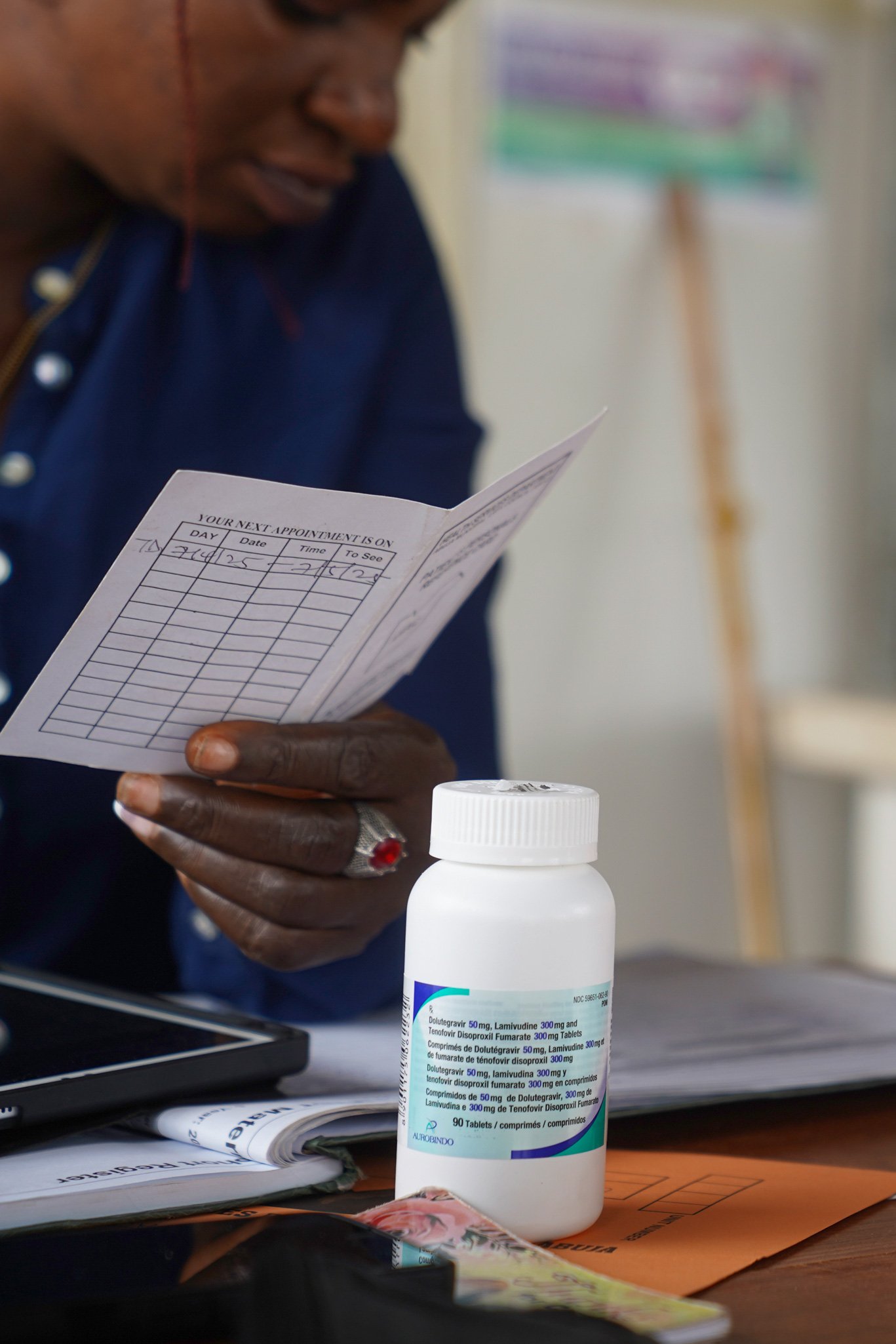
For John, the massive cuts in U.S. aid mean she no longer gets money to help pay for her transportation to go four miles from her home in Karonmajigi, a low-income suburb, to a hospital on the outskirts of the Nigerian capital of Abuja that has been supplying her with HIV-related medications.
Advertisement
She had earlier feared massive foreign aid spending reductions by the Trump administration and had asked doctors during her last visit to give her an extra supply.


Advertisement

“That’s why I wanted them to give me two cans of drugs that could last for six months when I visited the clinic in March,” John said.
John is now among the vulnerable patients—including pregnant women and breastfeeding mothers—scrambling to get life-saving medications, especially AIDS-related drugs.
Other major health initiatives financed by the United States—combating malaria, polio, and tuberculosis, as well as providing family planning services—are also being slashed in Africa.
Already in Nigeria, about 28,000 health workers were laid off because of these cuts, according to the Nigerian Ministry of Health and Social Welfare.
Advertisement
Public health researchers at Boston University estimate that more than 520,000 adults and children will die worldwide because of the loss in money from the United States.
Last year, John said the Lugbe Primary Healthcare Centre was giving medicine supplies that lasted for six months. Not anymore.

“The clinic wanted to manage the drugs, and I understand it. But now, I am out of medication again,” John said.
Advertisement
“And I don’t have transport fare to the clinic.”
A round-trip ride to the clinic, Kyuntu says, costs N2500, about $1.60, but John said she cannot afford it because she does not have a steady income and that she has three children to care for.
Advertisement
After President Donald Trump cut U.S. foreign aid, patients can no longer get a six-month supply of antiretroviral drugs. Now they can get at most three months’ worth of medications.
The result: Pregnant women and breastfeeding mothers in Nigerian communities struggle to get needed medical care.
Advertisement
Financial realities for poor mothers
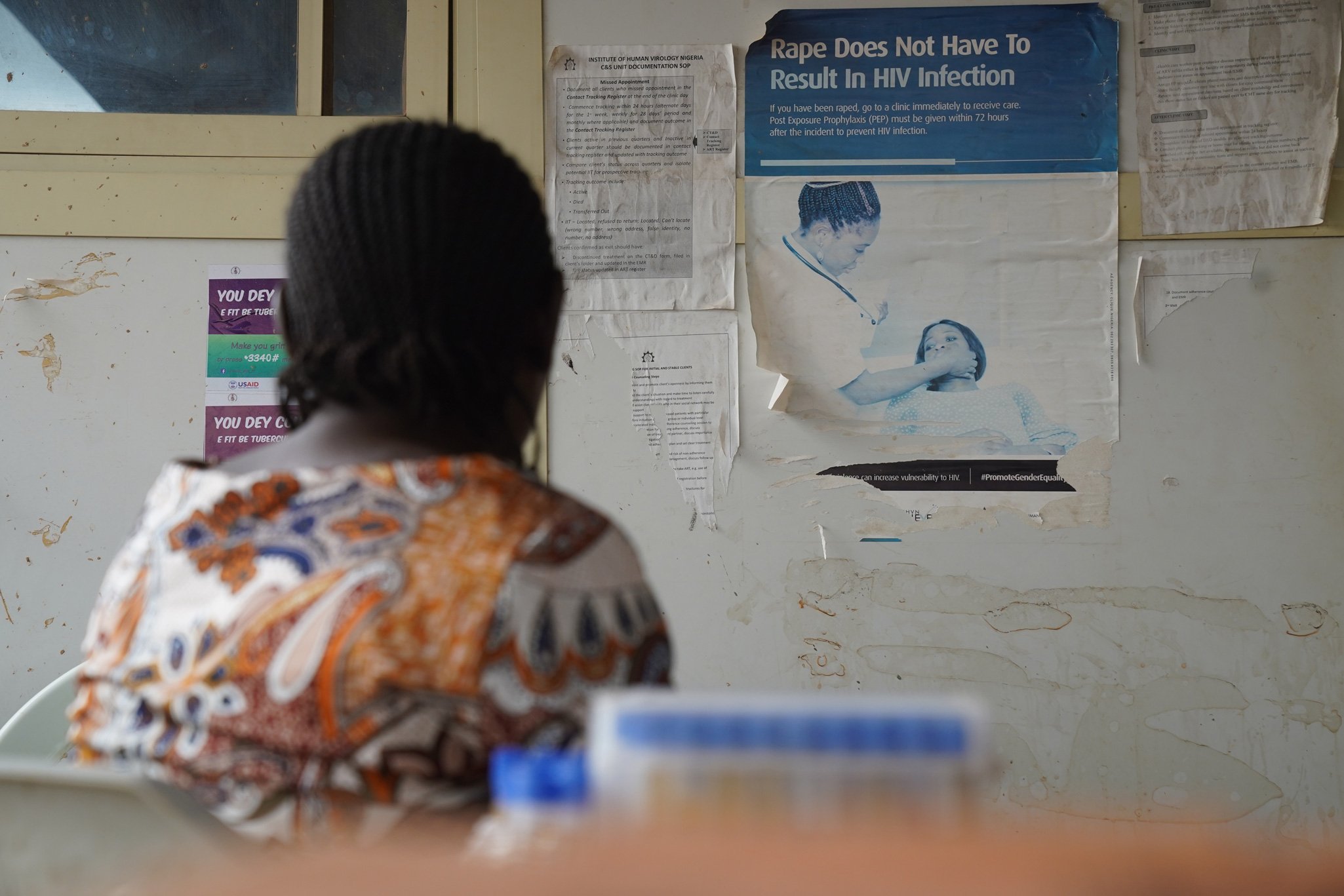
Esther Ina recently made a 40-minute walk to the antiretroviral therapy clinic at the Lugbe Primary Healthcare Centre in Abuja with the baby on her back. The 25-year-old said she had completed that journey twice in the past six months to get the drugs necessary to combat AIDS.
Two years before, she did fewer trips and spent less on transportation to get her needed medications.
Advertisement
“There are many other women under my supervision, like Ina and John, who are struggling in the same way,” says Tina Amos, a counselor at the clinic.

“Since the cycle was reduced from six months to two months, the complaint about the cost of transportation has increased, and women very often miss their appointment dates,” she said.
“When they come around or you call them to ask why they missed their appointment, they will tell you, ‘no money for transport.’ Occasionally, I listen to their lament, and I am compelled to pay for their transportation,” Amos said. “Many of these women are either unemployed or are without a stable income. It is difficult for them.”
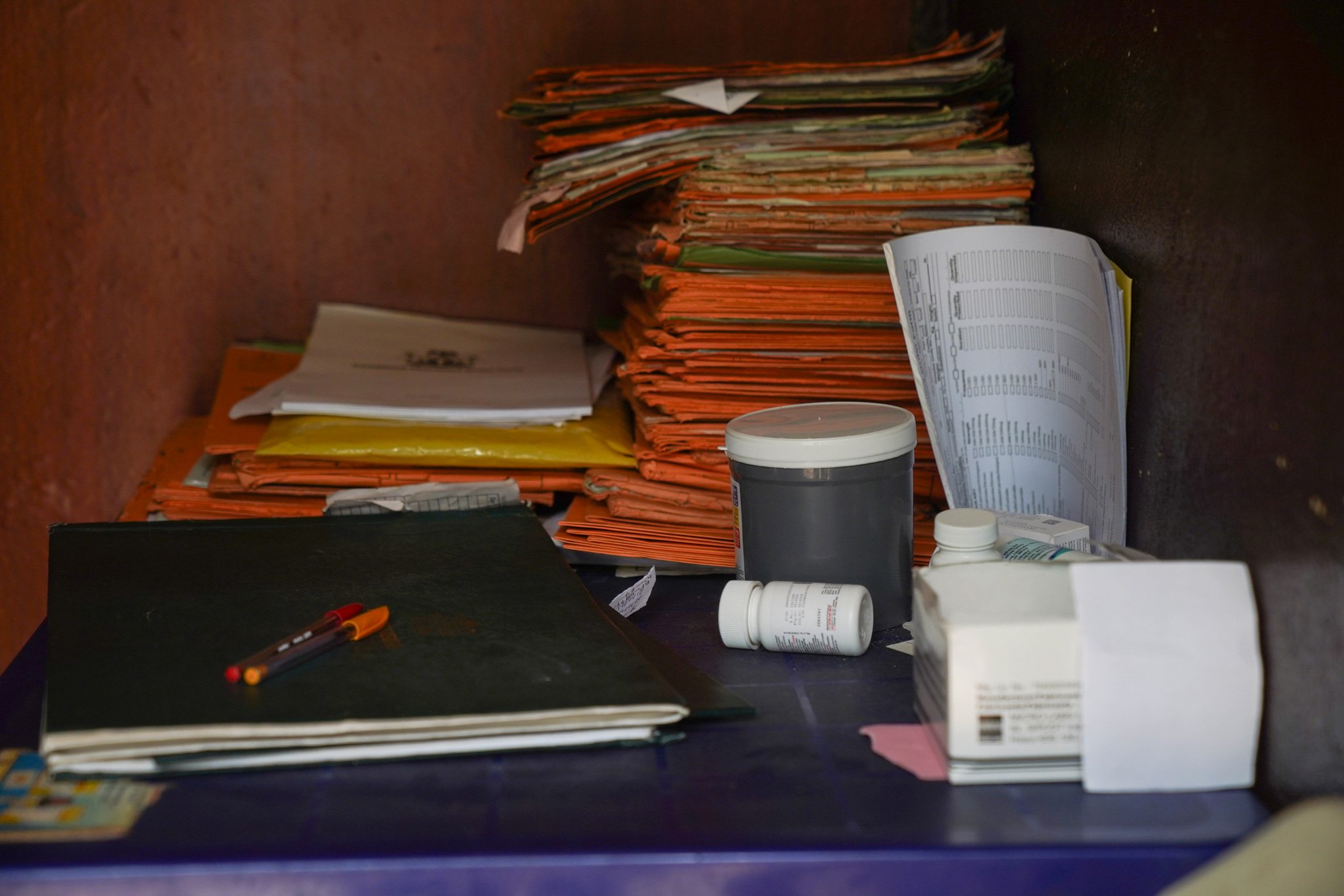
The Centre for Collaborative Investigative Journalism, CCIJ, interviewed six health professionals who asked that their names not be published because they were not authorised by their employers to speak to the press. They said patients are not getting needed drugs, and medical workers are overworked.
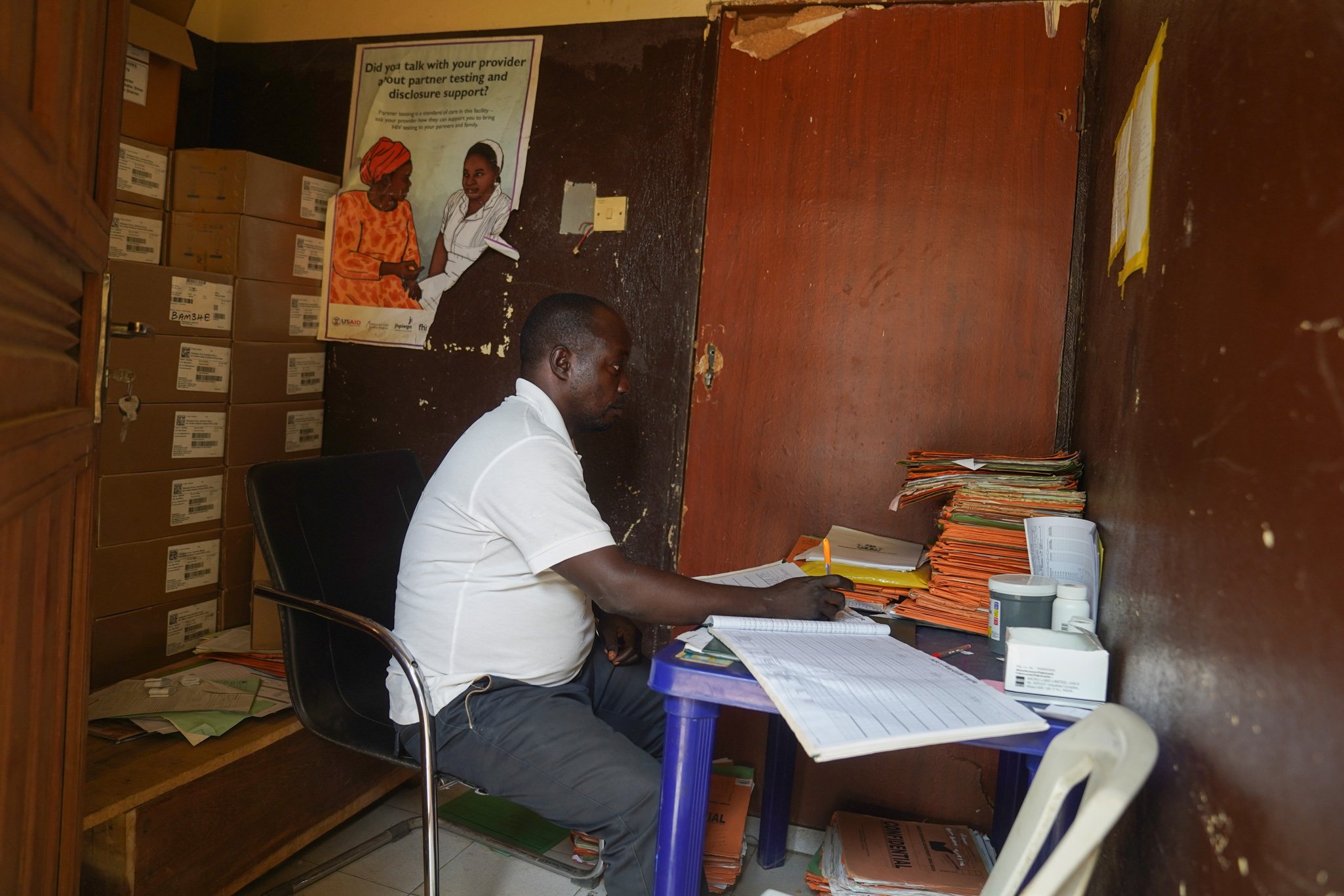

Frontline health workers now have to see patients more often—not for any special medical attention, but because they need to get refills for medicine more frequently. This takes away appointment slots that could be used for other patients with pressing medical needs. Layoffs following U.S. foreign aid cuts have also increased the workload for the healthcare workers who remain.
Setbacks in treatment
Before 2020, HIV patients could only get antiretroviral drug refills once a month. Patients who could not come in monthly were skipping dosages of life-saving medication.
Health professionals responded by advocating that drugs be dispensed to cover dosages for several months at a time. The advocacy led to changes. In 2020, medical facilities began supplying each patient with three-month antiretroviral refills. In 2022, that was extended to six months.
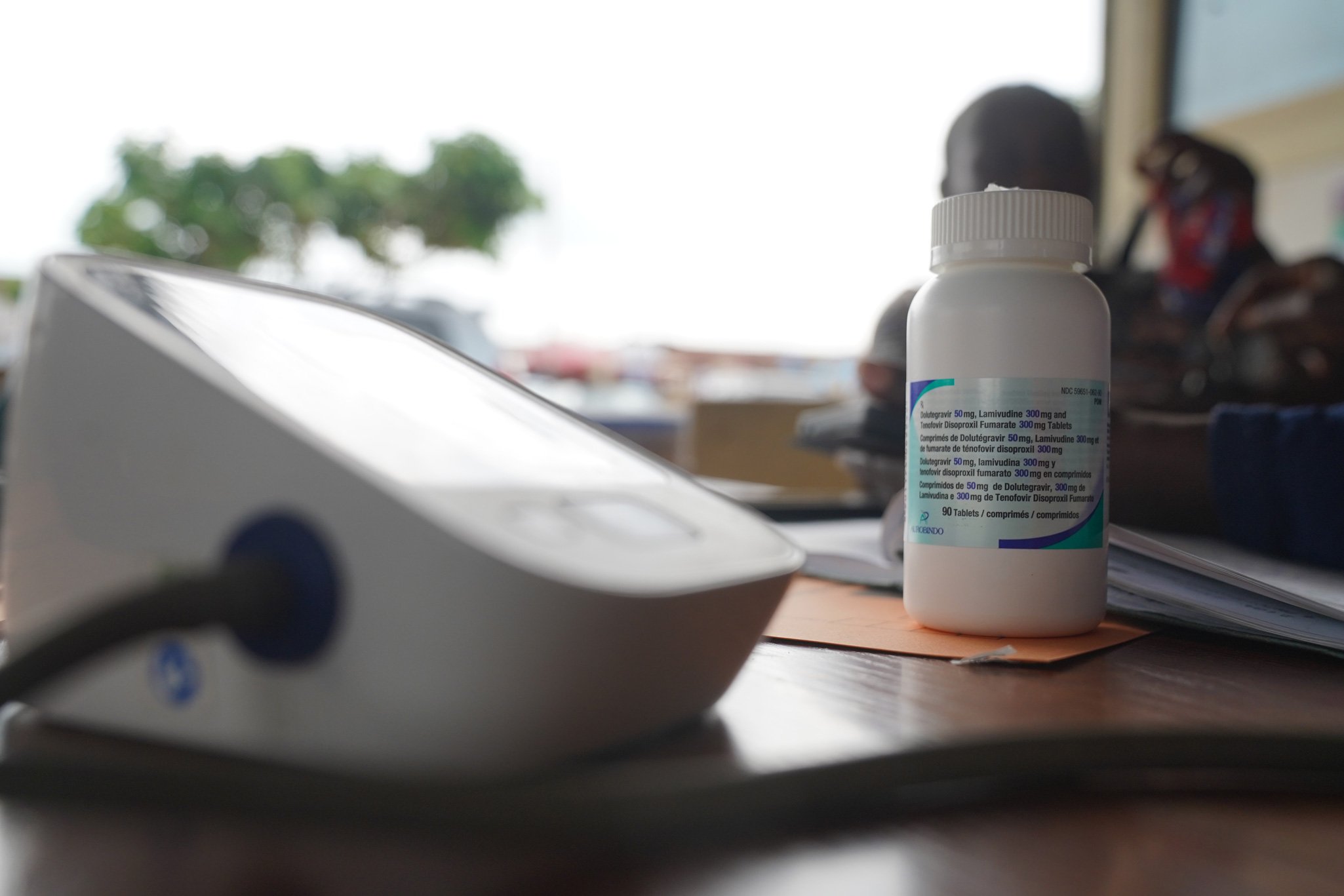
The Civil Society Networks on HIV and AIDS in Nigeria said the shift helped improve patients’ access to medical care and reduce the strain on frontline health workers, who were often required to attend to dispensing medications while juggling more pressing medical concerns.
In Nigeria, the cost of living has tripled in the past five years, driven in part by the economic reforms of President Bola Tinubu, including the removal of fuel subsidies. Fluctuations in Nigeria’s currency, the naira, along with rising inflation, have increased transportation costs, like those faced by John.
At the same time, women living with HIV often register for medical care at health facilities far away from their communities. The reason for this is their fear of identification and stigmatisation in their hometowns. They depend even more on longer-distance transportation to get medication.
Patients now skipping medications
The problems of getting medications to those with HIV have been made worse because of earlier drug shortages and the need for healthcare workers to manage a limited supply.
Pregnant women told CCIJ that they now skip doses to prevent running out of supplies.
“I skipped my doses in February, after I went to the health centre in Gwagwalada, on the outskirts of Abuja, and found that I couldn’t get drugs,” said Blessing Christopher, who was pregnant. “I was running out of medication.”
“I take today; I don’t take tomorrow. That’s how I was alternating the drugs to make them last longer,” she said.
Although the women said it is a necessary compromise, health experts warn that inconsistent use of antiretroviral drugs poses serious risks—both for the mother’s health and the baby’s well-being.
Deborah Ubieko, a medical doctor at the University of Abuja Teaching Hospital in Gwagwalada, finds this development concerning.
In all, Nigeria estimates that more than 2 million people are living with HIV in the country.
The Nigerian Minister of State for Health and Social Welfare, Iziaq Adekunle Salako, said more than 9,000 new pediatric HIV infections are recorded each year.
UNICEF stated in 2022 that progress in HIV prevention and treatment for children and adolescents in Nigeria “has nearly flatlined over the past three years” with limited access to diagnosis and care.
Nigeria has relied on U.S. dollars to fight AIDS
More than two decades ago, under President George W. Bush, the United States created the U.S. President’s Emergency Plan for AIDS Relief, known as PEPFAR, as a bipartisan program to combat AIDS and HIV around the world.
The U.S. embassy in Nigeria on its website lists PEPFAR as the major source of funding for HIV treatment in Nigeria. It has covered 90 percent of the country’s treatment programs, according to Nigeria’s National Agency for the Control of AIDS, known as NACA.
Data reviewed by CCIJ shows that between 2015 and 2024, the U.S. disbursed an average of about $270 million annually to support Nigeria’s HIV response efforts, mostly through PEPFAR.
Between 2003 and 2024, PEPFAR contributed over $6 billion to Nigeria’s HIV response. The funds were channeled through a network of international and local non-profit organizations and NACA. PEPFAR is still an active U.S. program, but its level of funding is unclear.
Aaron Sunday, leader of the Association of Positive Youths with HIV in Nigeria, a body that advocates for the rights and welfare of young people living with HIV, said Nigeria depends heavily on foreign aid to combat AIDS.
The U.S. cuts have caused a shortfall in drug supply in Nigeria and weakened the quality of services.
States with a high population of people living with HIV, such as Akwa Ibom and Benue, including the Federal Capital Territory, Abuja, have been struggling to cope with the overwhelming demand for care and limited resources to meet it, according to George Tsafa, a program assistant under the Institute of Human Virology in Abuja, which works to improve health services, research, and access to care in West Africa.
Multiple sources told CCIJ that HIV clinics and research organisations across several Nigerian states, including Akwa Ibom, Sokoto, and Plateau, were shut down earlier in the year and have since reopened at a reduced capacity.
The Trump administration’s cuts have led to the closure of many HIV clinics in Plateau State. Healthcare workers lost their jobs. Clinics have reopened but work at a lesser scale, according to Chris Damcher, chairman of the Plateau Civil Society Organisation Forum.
In Kebbi, U.S. assistance was the major source of funding for medical care, according to Danjumma Sanchi, spokesperson of the Kebbi State Contributory Healthcare Management Agency.
“The state heavily relied on them for funding, and when that was cut short, service dropped significantly,” he said.
“As it stands, a lot will depend on the state and federal government. They have to do something and do it urgently. If not, the population will suffer,” according to Sanchi.
Children no longer getting needed drugs
Benue State has the second-highest population living with HIV in the country, according to data provided by NACA to CCIJ. It is a state with a high need for antiretroviral medications.
Happiness James, 32, heard that clinics in Benue had stopped giving out drugs and did not know what to make of the news.
“If they start selling, I cannot afford it. It felt like my life was over, and all I could do was cry,” she said.
She became worried when the supplies of HIV medicine grew scarce at the Comprehensive Health Clinic in the Gboko Local Government Area and was more apprehensive when Septrin, the antibiotic prescribed to protect her five-month-old baby, was no longer available at the clinic.
Septrin is a crucial medication for HIV-exposed infants with weak immune systems to prevent pneumonia, malaria, and other ailments.
Nurses now tell her to buy the drug at the pharmacy, which costs about N2,500 monthly, about $1.40 in U.S. dollars.
Although not nearly as expensive as antiretroviral drugs, James and many other women still struggle to afford the expense.
Deborah Nongom, a breastfeeding mother residing in Rice Mill, a small community in Benue, has also been struggling with the cost of drugs, sometimes having to choose between purchasing medication and other essentials for her family.
“I just want things to go back to how they were before,” she said. “It was better then, much easier. I am praying for more drugs to be supplied because that is what is keeping me and the baby safe.”
Esther Alkali, a healthcare worker at the clinic, said the facility has not been resupplied with Septrin, so it can no longer dispense the drug to patients.
“There are no drugs for children anymore,” she said. “I have tried to find out why, but no response. Parents have to buy themselves now, and sometimes, the women will complain that they don’t have the money or can’t find it.”
Test kits become harder to get
In addition to medications, other essential medical supplies are becoming scarce.
Joseph Grace, a health worker at the PHC in Ichwa, Makurdi, said the volume of medical supplies delivered to the facility has steadily declined since the start of the year. Each new shipment arrives with fewer items than the last.
As essential medical commodities become less available, frontline health workers find themselves struggling to provide care.
Test kits, for instance, are harder to get. The health clinic in Gboko has been unable to do HIV tests on pregnant women, except for those who were able to get testing kits from elsewhere.
According to Alkali, pregnant women who come in for their first visit are typically required to undergo routine HIV screening. But with test kits out of stock, the clinic has had to turn many of them away or ask them to return at some later date when she hopes testing kits will become available.
She said only those who can buy test kits from pharmacies are tested.
But that is not possible for many women.
“Many of them travel long distances from remote villages, and they always come back saying they couldn’t find the kit,” she said.
Alkali said on average, the clinic registers around 170 pregnant women each month. That means the lack of testing kits has serious health implications for many women.
Frontline health workers in the state say they have been overwhelmed by patients’ needs since once-routine health programs have been discontinued, including providing antiretroviral medications to those exposed to AIDS but who have not tested positive.
These cuts include ending pre-exposure prophylaxis and post-exposure prophylaxis, two major antiretroviral prevention programs offered to individuals at high risk of infection, including survivors of sexual assault, sex workers, and partners of people living with HIV.
This affects pregnant women and breastfeeding mothers, according to Kate Korave, director of the HIV Testing Service in Gboko, in Northcentral Nigeria
“Everything changed” after the Trump administration’s policies, she said. “And the changes were drastic.”
Funding gap in treatment
To bridge the funding gap created by the U.S. spending cuts, the Nigerian government began in February to allocate additional funds to HIV treatment.
The Federal Executive Council approved N4.8 billion, the equivalent of $3.1 million, for HIV treatment. The money is coming from the World Bank and other international sources.
The Nigerian Senate allocated an additional N300 billion, about $200 million, to the health sector in the 2025 budget for health programs, including combating HIV.
The National Agency for the Control of AIDS announced plans to begin producing HIV-related supplies, including test kits and antiretroviral drugs.
But these efforts are far below the roughly $270 million in average annual funding that Nigeria received from the U.S. for combating HIV over the past decade, according to the CCIJ’s data review.
Health workers and nonprofit organisations in Nigeria who once partnered with USAID for HIV treatment say the country’s progress in controlling the virus is at risk.
Aaron Sunday, the APYIN director, described the situation as a lesson for Nigeria to prioritise domestic funding for life-threatening diseases.
Nigeria, he said, “has to scale back its dependence on foreign assistance.”
Rimamnunra Grace, head of the Aids Prevention Initiative in Nigeria (APIN), a non-profit providing HIV care in Benue State, said that means Nigeria needs to buy more needed drugs.
“The most important thing is that we pick up on the procurement of the drugs,” she said. “That’s where the work is. If that is not in place, then there is nothing we are doing.”
This story was supported by Nigeria Health Watch through the Cross-Learning and Africa Engagement component of the Global Policy Advocacy Project






