BY SYLVESTER OJENAGBON
It is believed that about 5 to 10 out of every 100 people in the world will get a peptic ulcer at some point during their lifetime. Although the number of people affected has decreased over the years due to factors like improved sanitation and hygiene, the number of new cases has remained high.
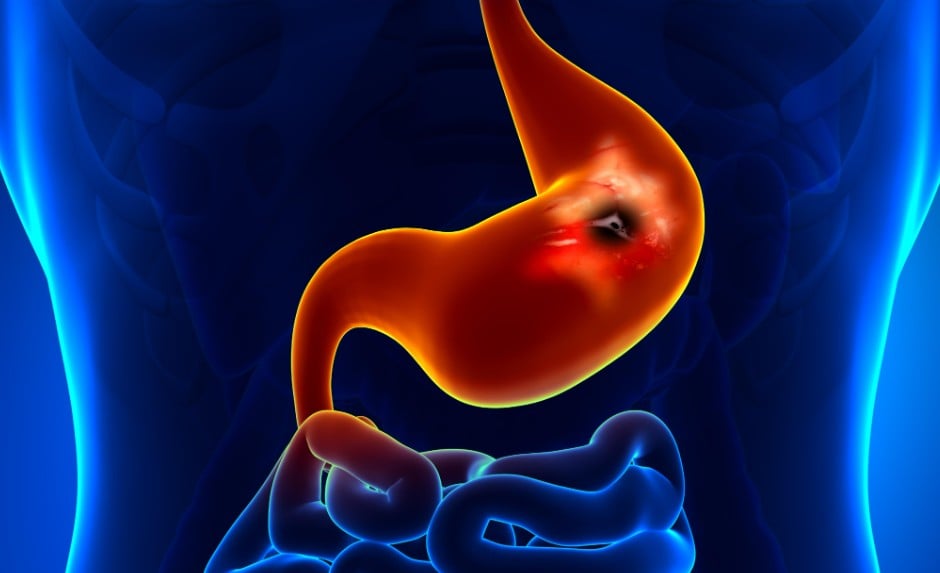
An ulcer is an open sore or lesion which occurs on the surface of the skin, mucous membranes, or lining of an organ. It is characterised by a loss of tissue, often involving inflammation and potential pus. Ulcers can occur in various locations, including the stomach, intestines, mouth, and skin.
A peptic ulcer, on the other hand, is an open sore that develops in the lining of the stomach or the duodenum (the first part of the small intestine). Although peptic ulcers and stomach ulcers are often used interchangeably, there is a subtle difference in their meaning. Peptic ulcers are a general term for sores in the lining of the stomach or the first part of the small intestine, while stomach ulcers (gastric ulcers) specifically refer to ulcers located within the stomach. In essence, all stomach ulcers are a type of peptic ulcer, but not all peptic ulcers are stomach ulcers.
Advertisement
Now, peptic ulcers are typically caused by either infection with Helicobacter pylori (H. pylori) bacteria or by long-term use of nonsteroidal anti-inflammatory drugs (NSAIDs).
Helicobacter pylori is a bacterium that lives in the stomach and can damage the lining, leading to ulcers.
It can disrupt the protective mucus layer in the stomach and duodenum, allowing stomach acid to erode the lining. This is a major cause of peptic ulcers.
Advertisement
Long-term or high-dose use of NSAIDs can weaken the protective lining of the stomach and duodenum, making them more susceptible to ulcer formation. Examples of NSAIDs include ibuprofen, aspirin, and naproxen.
And physical or emotional stress can temporarily disrupt the stomach lining and increase the risk of ulcers. Some medications, particularly those affecting acid production, can also contribute to ulcer formation.
Conditions where the stomach produces too much acid can equally lead to ulcers, but this is rare. Excessive alcohol consumption and smoking can also increase the risk of peptic ulcers. Furthermore, some people may have a genetic predisposition to developing ulcers.
Early symptoms of peptic ulcers can include a dull, burning, or gnawing pain in the upper abdomen, often between the belly button and the breastbone. This pain may come and go and might be worse when the stomach is empty.
Advertisement
Others are a feeling of fullness or discomfort even after eating a small amount of food; feeling sick to your stomach or vomiting, potentially with blood; a feeling of fullness or tightness in the abdomen; excessive burping; and a burning sensation in the chest, often associated with acid reflux.
Other possible symptoms include indigestion, loss of appetite, and, in some cases, unintended weight loss.
If you have any of these symptoms, it is best to consult with a healthcare professional for proper diagnosis and treatment. However, it is important to note that some people may not experience any symptoms; ulcers can be “silent”.
Poorly managed or untreated peptic ulcers can lead to serious complications. It can erode blood vessels, causing bleeding. This can lead to anaemia if the blood loss is slow and chronic, or shock if the blood loss is rapid and severe.
Advertisement
It can also erode through the stomach or intestinal wall, creating a hole (perforation). This allows stomach contents to leak into the abdominal cavity, leading to inflammation of the abdominal lining, infection, and potentially sepsis.
Ulcers in the stomach or duodenum, especially at the junction of the stomach and small intestine, can cause scarring and swelling. This can narrow or block the opening to the small intestine and lead to difficulty emptying the stomach, causing vomiting and malnutrition.
Advertisement
Although less common, chronic ulcers, especially those caused by H. pylori infection, can increase the risk of developing stomach cancer. An ulcer can similarly extend beyond the stomach or duodenal wall, penetrating other organs or structures in the abdomen, potentially causing inflammation or damage.
Peptic ulcers, in rare cases, can lead to other complications, such as gastrocolic fistula formation (an abnormal connection between the stomach and colon) or, in severe cases, even death.
Advertisement
To prevent peptic ulcers, it is important to avoid factors that irritate the stomach lining and increase the risk of infection. This includes managing stress, limiting alcohol consumption, quitting smoking, and being cautious with medications like NSAIDs. In addition, ensuring food is well-cooked and handled and maintaining good hygiene can help prevent infections like H. pylori, a major cause of peptic ulcers.
Peptic ulcer disease treatments focus on healing ulcers and preventing recurrence. While a specific “ulcer diet” may not be necessary, some people find that avoiding caffeine and spicy foods can help with symptoms.
Advertisement
Endoscopy may be used in some cases to stop bleeding ulcers or remove parts of the ulcer.
Although surgery is rarely needed for peptic ulcer disease, it may be an option in rare cases, where ulcers do not heal with medication or if there are complications.
Peptic ulcers can be painful and disruptive, but the power to prevent and effectively manage them largely rests in our hands. By arming ourselves with knowledge, embracing preventative strategies, and seeking timely medical intervention, we can significantly reduce the burden of this common ailment and foster a future of better gut health for all.
Ojenagbon, a health communication expert and certified management trainer and consultant, lives in Lagos.
Views expressed by contributors are strictly personal and not of TheCable.